What is Ochsner Health’s Neurosciences m3D lab, and what sets it apart?
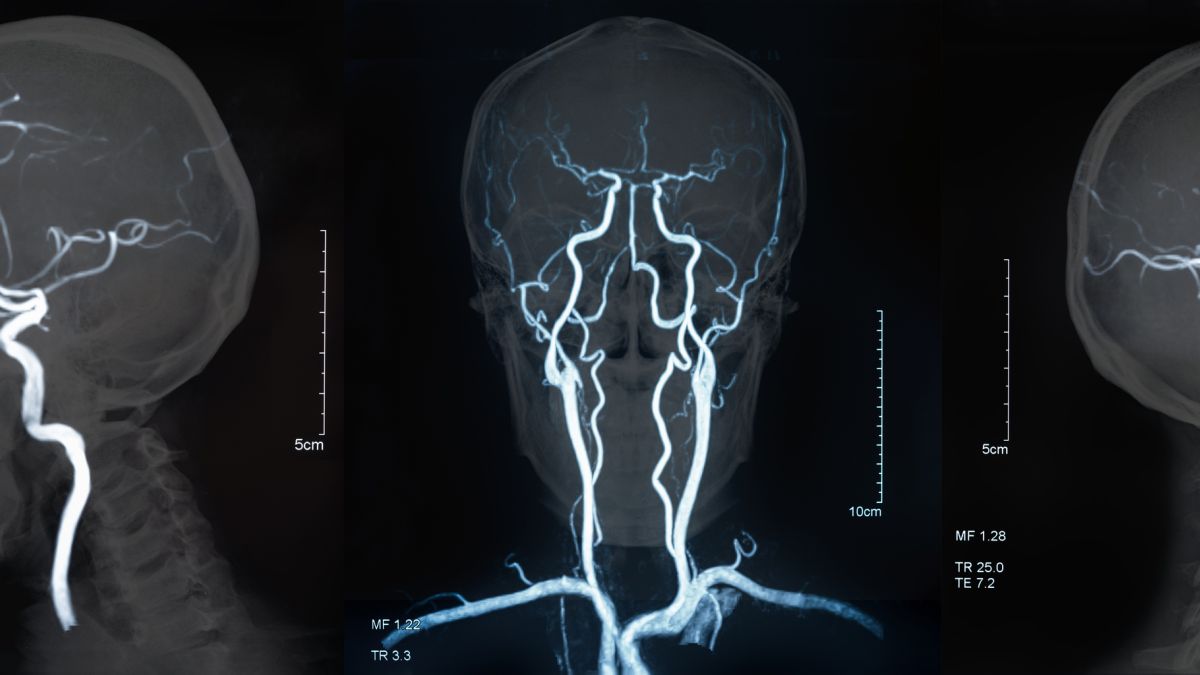
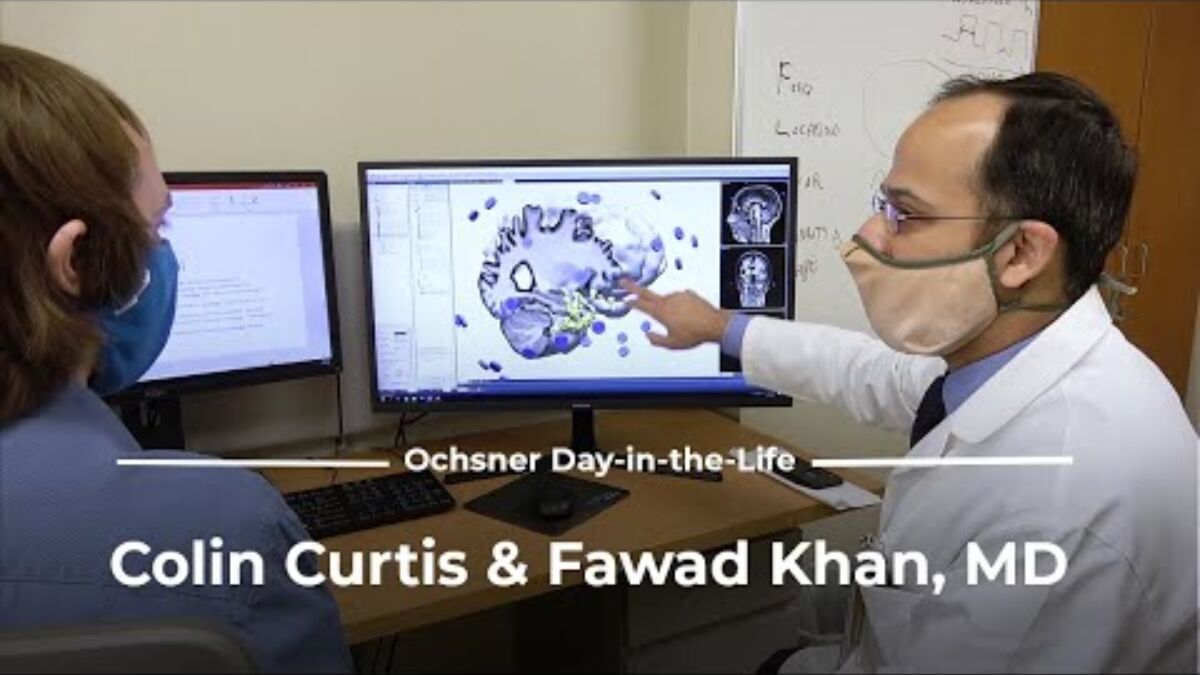
We live in a three-dimensional, or 3D, world, and our brains are built to process 3D information. Unfortunately, imaging and other important medical information often appears in 2D, challenging patients’ abilities to fully understand their diagnoses. That’s where the Neurosciences m3D lab, or medical 3D lab, at Ochsner Medical Center - New Orleans comes in. Serving patients from Louisiana, Mississippi and beyond, the Neurosciences m3D lab uses leading-edge technology to create 3D models from patients’ 2D imaging, along with other tools for patient education.
The Neurosciences m3D lab brings together specialists in neuroscience, neurology, biomedical engineering and software development to collaborate with doctors on state-of-the-art solutions. Other health systems may have a neuroscience laboratory or research labs, but the Neurosciences m3D lab’s deep integration into patient care is what sets it apart. The lab’s team uses 3D printing, virtual reality and augmented reality to create personalized tools that enhance patients’ understanding of their medical conditions. Every day, our Neurosciences m3D lab helps bring greater understanding to medicine while pioneering its future.