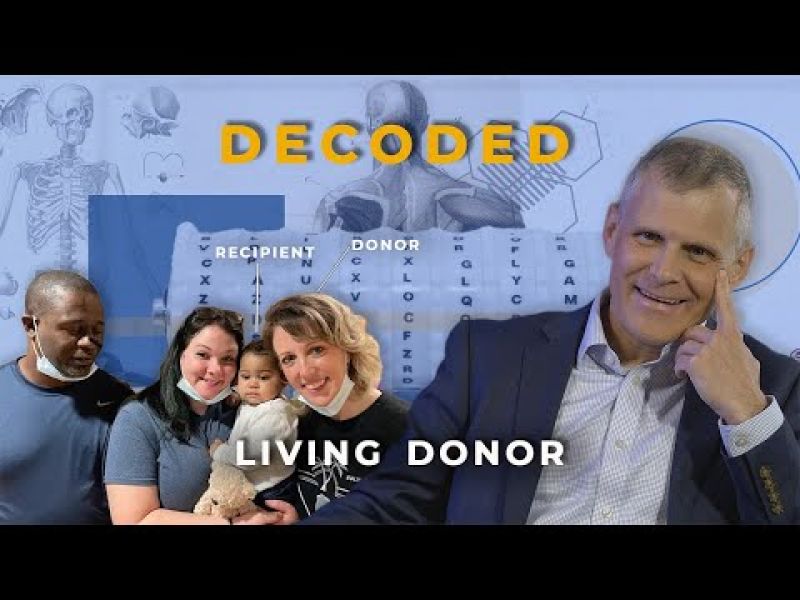
Why choose Ochsner for a living donor liver transplant?
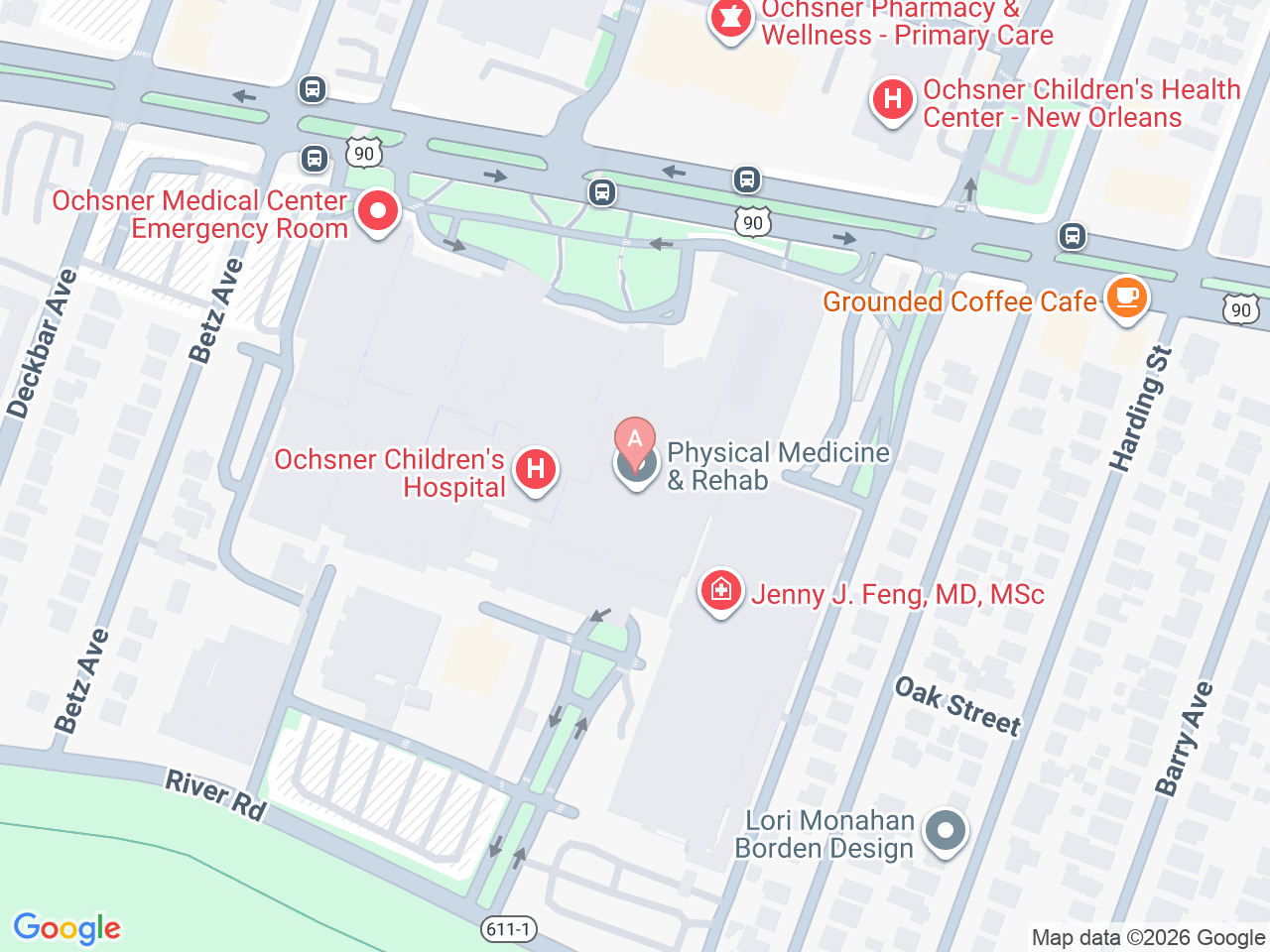
At the Ochsner Transplant Institute in New Orleans, Louisiana, we bring hope to patients and their families through our living donor liver transplant program. As the only program of its kind in the state and the only active living liver transplant program in Louisiana, Ochsner Health is proud to deliver nationally recognized, compassionate and high-quality care.
Each year, over 1,400 people in the United States lose their lives waiting for a liver transplant. By offering living donor liver transplants, we provide a faster, life-saving alternative, underscoring our unwavering commitment to saving and transforming lives.
Our expert surgeons tackle some of the most complex cases, including re-transplantation, transplants for obese patients and those with portal vein thrombosis. With extensive experience in split liver transplants, reduced-size liver transplants and living donor liver transplants for both adults and children, our team is equipped to handle the most challenging scenarios.
From your first step in the process, you’ll be supported by a dedicated team of specialists, including transplant hepatologists, liver transplant surgeons, living-donor coordinators, advocates, social workers, nutritionists and financial advisors, all working together to guide you through every stage of your journey.
Ready to take the first step toward becoming a living liver donor? Complete the Living Liver Donor Contact Form.