Why Choose Ochsner Health for Urologic Oncology Care?
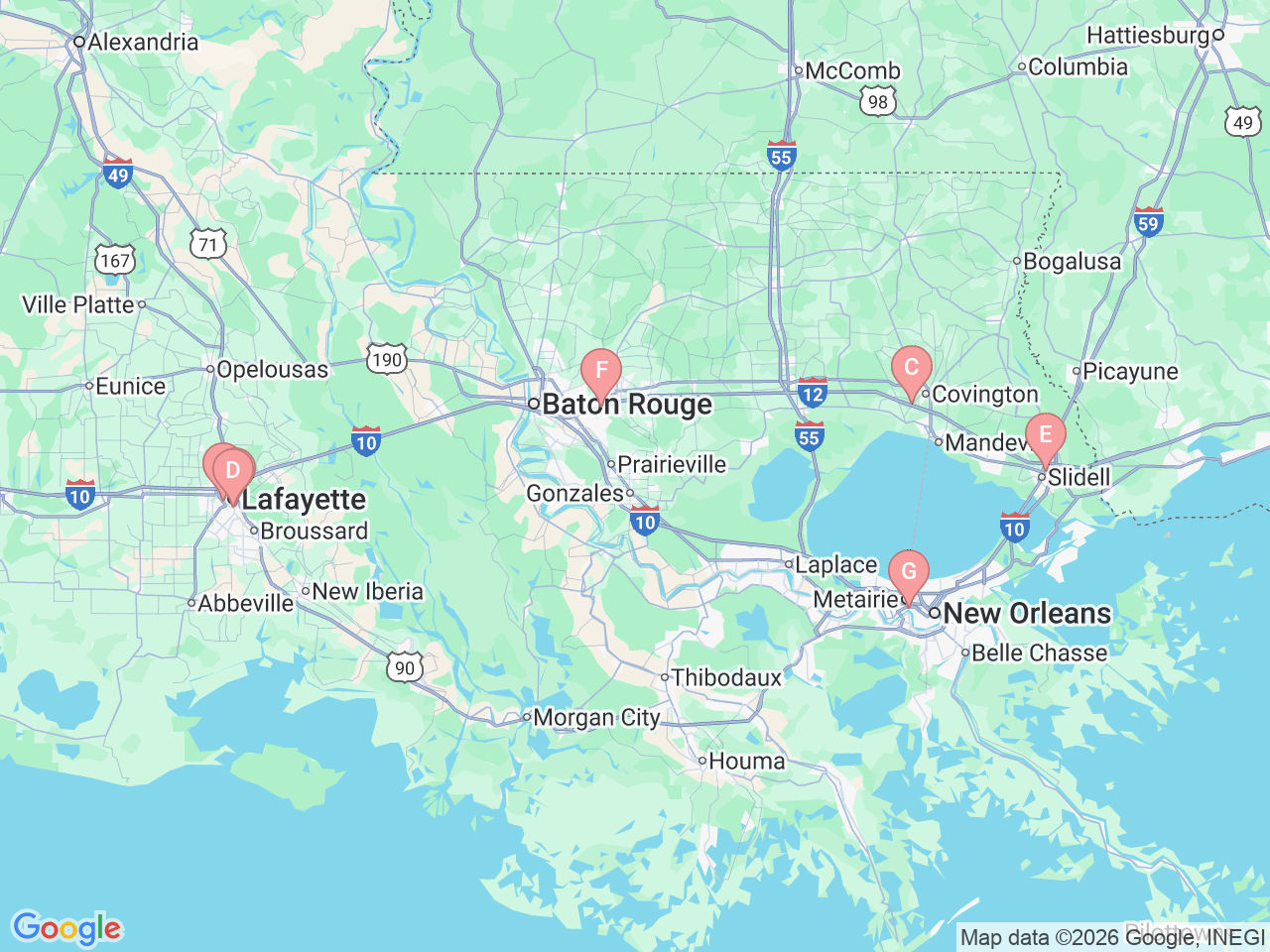
Ochsner Health provides comprehensive genital and urinary organ cancer care in New Orleans, Covington, Slidell, Baton Rouge, Lafayette and Shreveport, Louisiana. Our urologic oncology team works closely with other doctors and providers to offer personalized care and treatment plans.
We have resources for patients including mental health services, nutrition guidance, support groups and genetic counseling.
As a major referral center, we specialize in advanced medical care for complex urologic cancer conditions. Our surgeons help patients manage all aspects of their prostate cancer care in one location.
We are one of the few centers in the Gulf South that provides a full range of prostate cancer treatments, all in one place, ensuring you receive comprehensive and coordinated care.