Why choose Ochsner Health for neonatal intensive care?
Babies born prematurely or with serious health problems need specialized care and support for a successful start to life outside the womb. That’s exactly what they receive throughout Ochsner’s network of neonatal intensive care units, or NICUs, in Louisiana and Mississippi. When your baby enters a neonatal intensive care unit, they’ll receive around-the-clock care from a multidisciplinary team of experts until they’re healthy enough to go home with you.
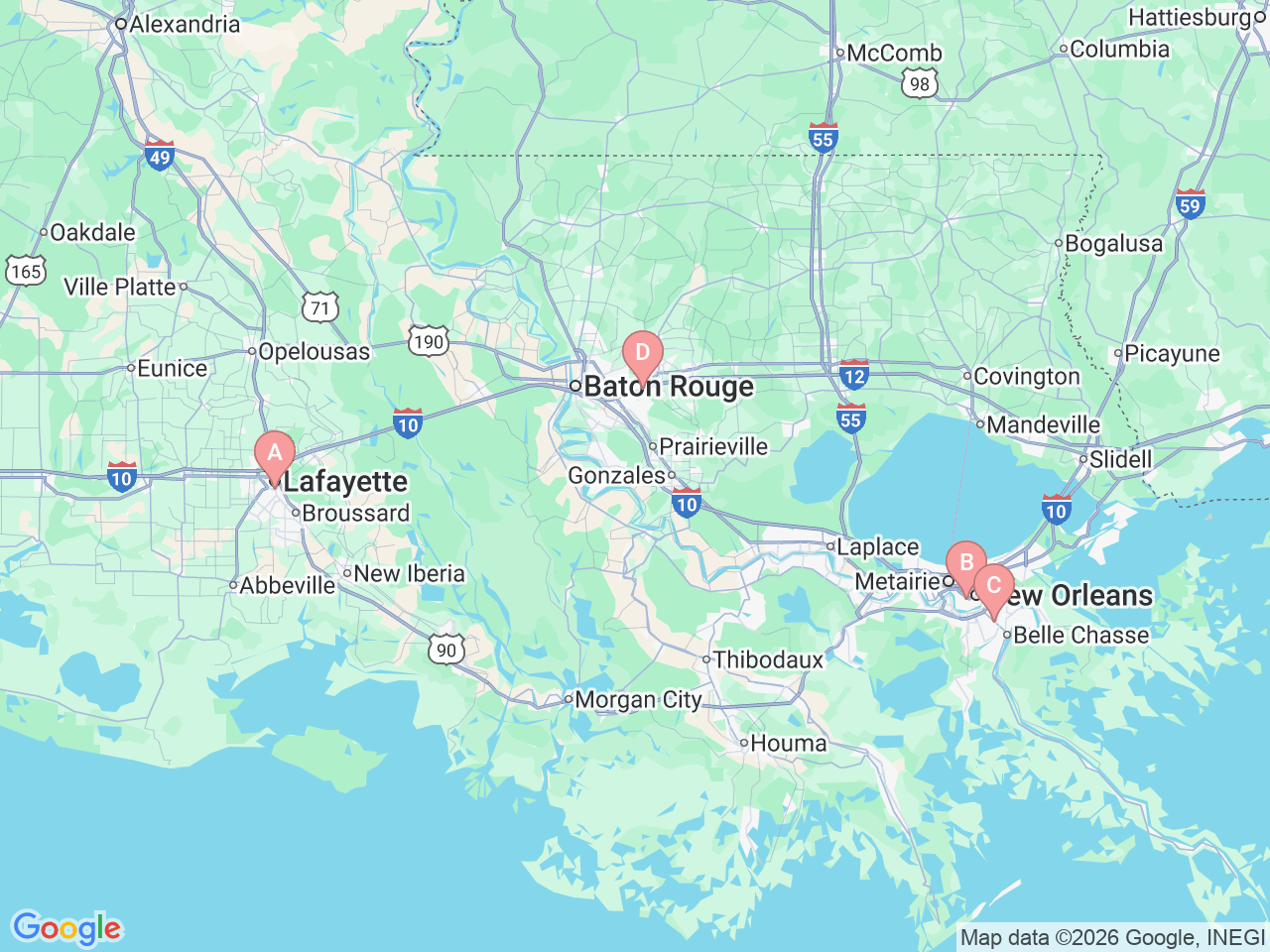
Our neonatal intensive care units are equipped to offer varying levels of medical care to premature babies based on their gestational age (how long they have been in the womb) and health status. If your baby needs a higher level of care than your local Ochsner hospital provides, we’ll transfer them to another NICU in our system. Our flagship, 54-bed neonatal intensive care unit at Ochsner Baptist Women’s Pavilion in New Orleans offers access to leading-edge treatment technologies and the full range of pediatric specialists and subspecialists through nearby Ochsner Children's Hospital.
Whether your baby is receiving care in the neonatal intensive care unit at Ochsner Baptist Women’s Pavilion or one of the other NICUs in our network, they have the expertise and services of our entire health system behind them.