Why choose Ochsner for cerebral amyloid angiopathy treatment?
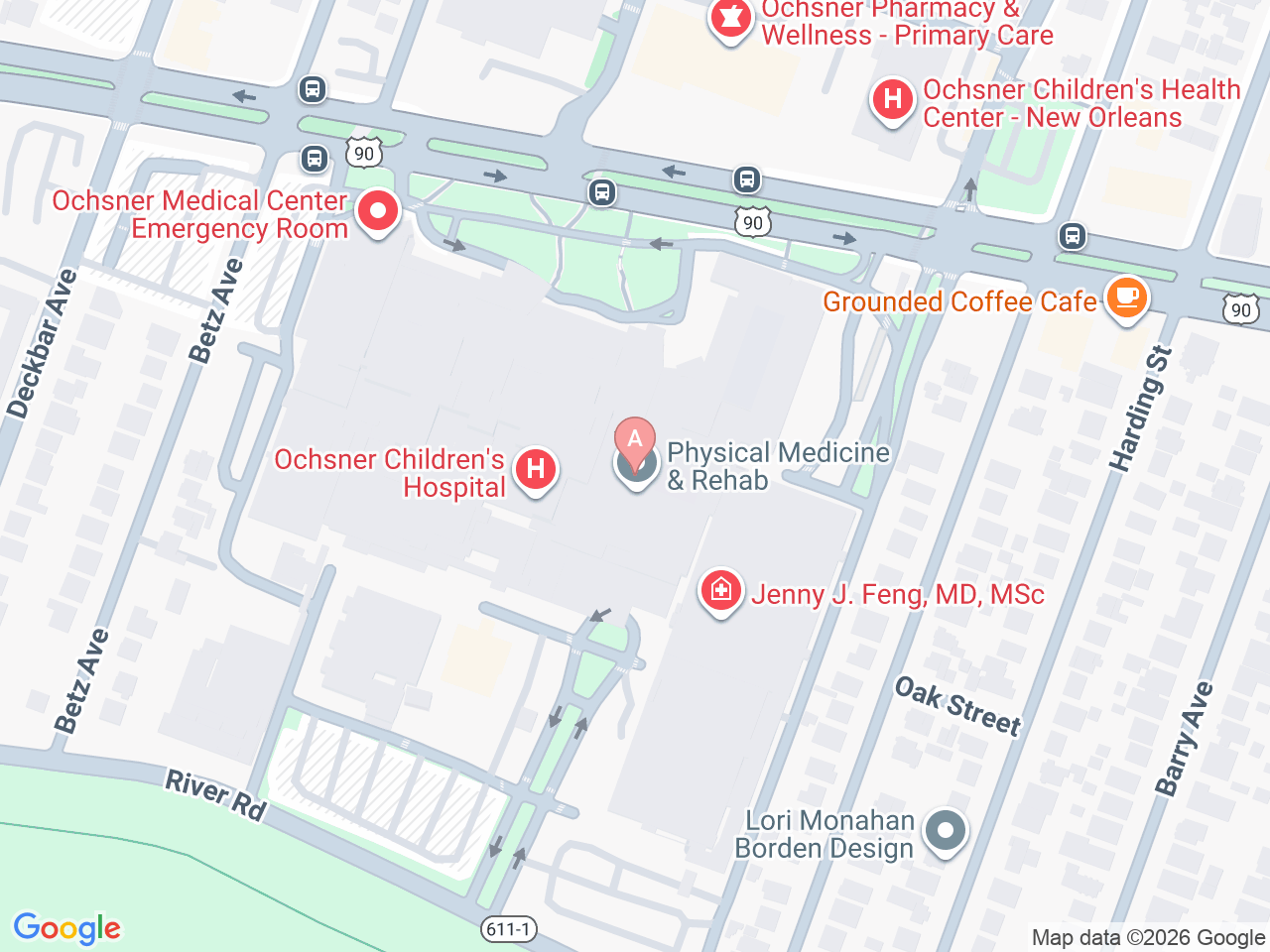
At Ochsner, we offer a dedicated clinic in New Orleans, Louisiana, specifically for people with cerebral amyloid angiopathy (CAA).
We bring together experts who specialize in brain blood vessels and specialists who focus on memory and thinking challenges. Our goal is to continually develop better treatments for CAA and enhance the quality of life for our patients.
Cerebral amyloid angiopathy (CAA) is a condition where a sticky protein called amyloid-beta builds up in the small blood vessels of the brain over many years. This build-up can weaken the blood vessels, making them more likely to leak and cause tiny bleeds in the brain that often go unnoticed.
Over time, these small changes can impact memory and cognitive function. In some cases, a blood vessel may burst, leading to a larger bleed and more serious symptoms, like a stroke.
Email our clinic at caa@ochsner.org to schedule a consultation.