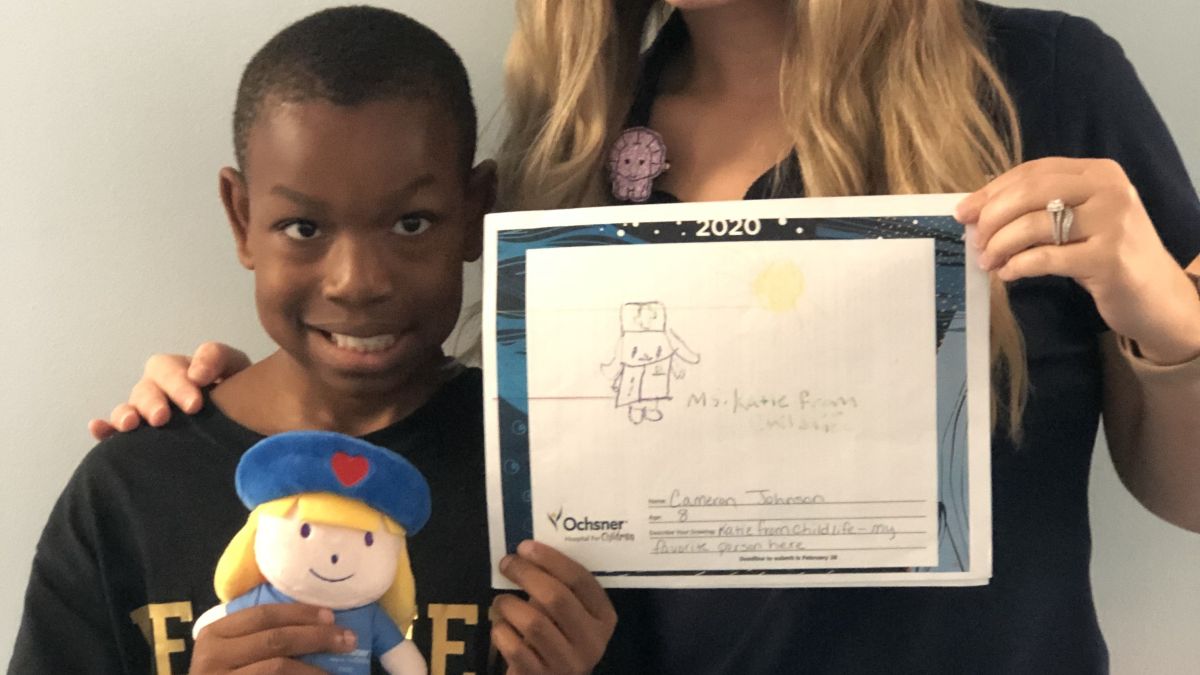
Why Choose Ochsner Health for Child Life Services?
At Ochsner Children's Hospital in New Orleans, Louisiana, our Certified Child Life Specialists are here to help children and their family members minimize stress associated with the healthcare experience. Our team of Child Life Specialists promote family-centered care by helping kids and families understand the plan for treatment and giving them tools to reduce fear and anxiety while supporting their individuality, strengths and mechanisms for coping.
Our Certified Child Life Specialists hold advanced degrees in areas related to child growth and development. They are specially trained to provide age-appropriate information to help children prepare emotionally and increase their ability to cope with all aspects of the medical environment during a hospital stay. Through education and therapeutic play opportunities, we promote resiliency and help normalize an environment that may feel intimidating.