Why choose Ochsner Health for your female pelvic healthcare?
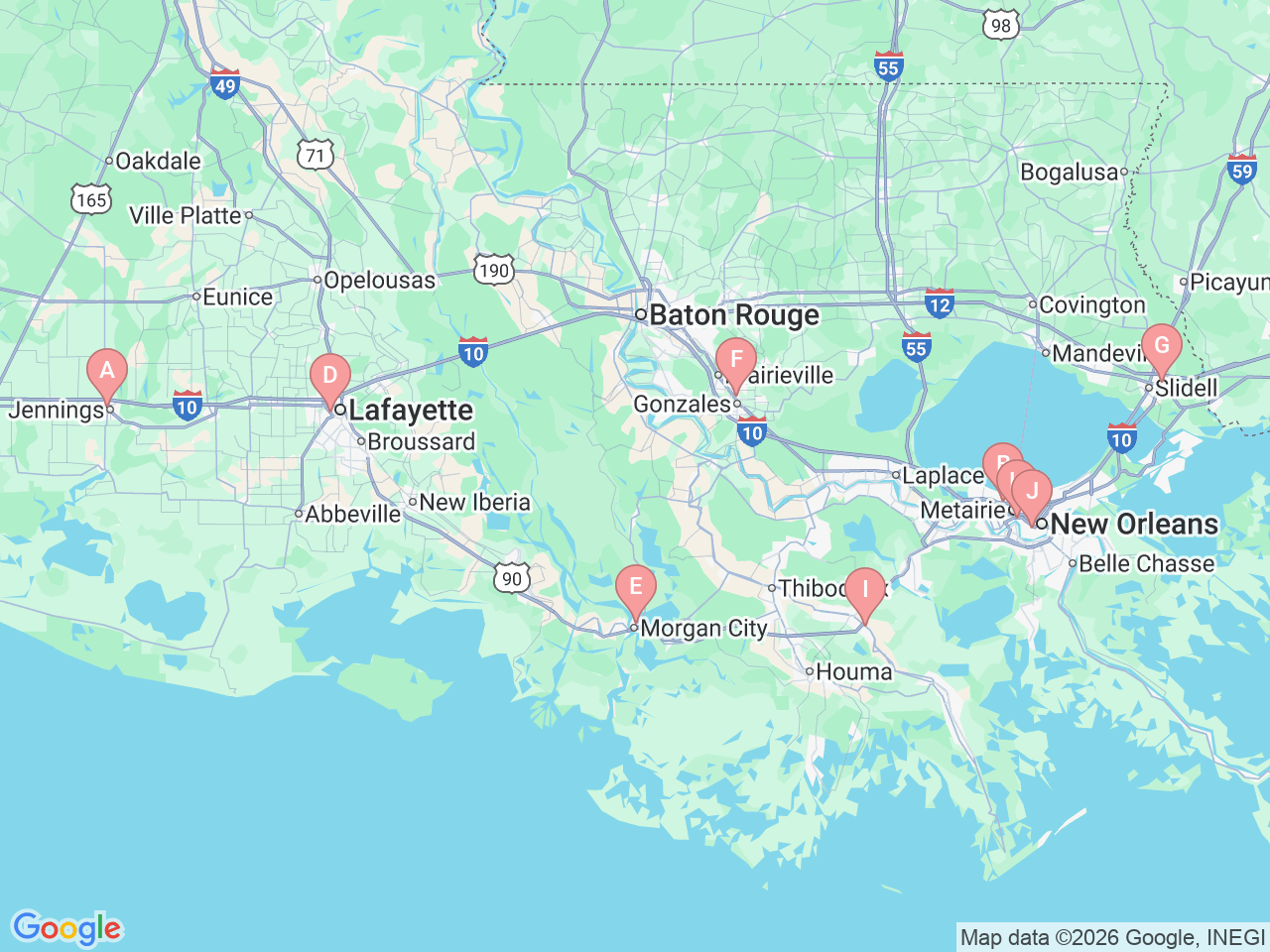
Ochsner provides expert pelvic healthcare with locations in New Orleans, Metairie, Lafayette, Jennings, Morgan City, Raceland, Gonzales and Slidell, Louisiana. We specialize in comprehensive care for pelvic floor issues and other pelvic health conditions, offering services that are unmatched in the region. Our program is built on a foundation of high-quality care, continuous innovation, and exceptional patient outcomes. Ochsner Baptist has earned accreditation from the Surgical Review Corporation as a Center of Excellence in Continence Care for Women, a recognition of our commitment to delivering outstanding care.
When you come to our pelvic floor center, you are paired with a nurse navigator who will help match you to the team members and services that best fit your condition and needs. Based on your needs, your care team may include fellowship-trained surgeons, physicians, nurse practitioners, physician assistants, physical therapists or specially trained nursing staff.
We also offer dedicated clinic hours for patients who need to see specialists in both the pelvic health program and the colon and rectal surgery clinic. This partnership allows patients to meet with both teams on the same day, decreasing the number of appointments and improving collaborative care.
To help you get the care you need and ensure continuity of care, the specialists in the female pelvic health clinic also work closely with experts in other Ochsner departments, including: