Why choose Ochsner Health for your nephrology care?
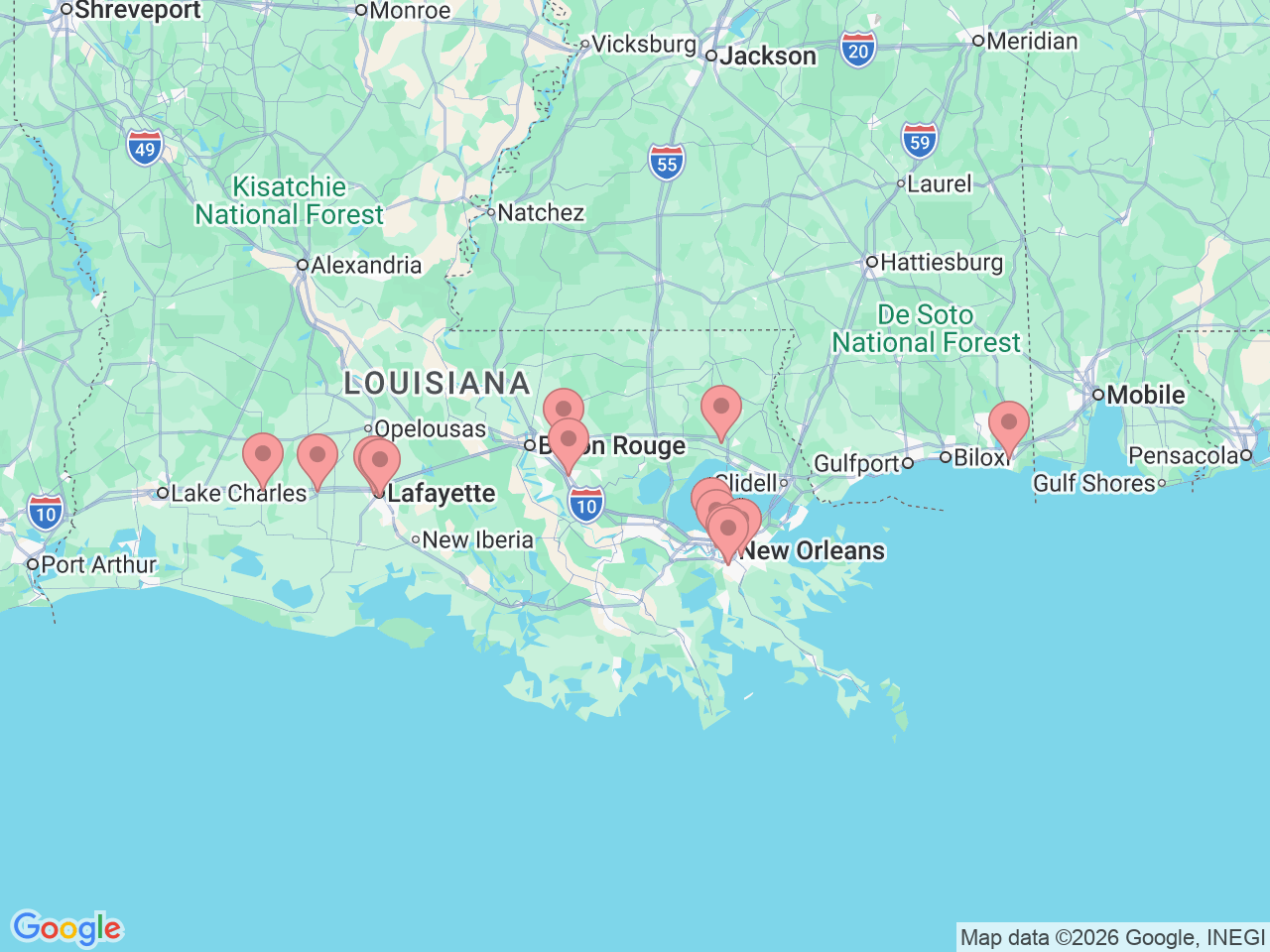
Ochsner’s nephrology team provides advanced kidney care for patients in Covington, Lafayette, Jennings, Crowley, Baton Rouge, Prairieville, New Orleans, Metairie, Jefferson, Marrero, Louisiana and in Pascagoula, Mississippi. U.S. News & World Report recognized our comprehensive program as “High Performing” in kidney failure care, placing us in the top third of ranked programs nationwide.
We are a trusted leader in kidney health. Our providers offer initial diagnosis, second opinions and a full range of treatments. We focus on you as a whole person, not just your condition. To support your overall well-being, we provide:
- Exercise programs for patients receiving dialysis
- Case management or nurse navigator assistance to guide your care
- Education programs for those with stage IV chronic kidney disease or end-stage renal disease
- Nutritional counseling from specialized renal dietitians
Depending on your condition and needs, we may also offer virtual visits to make care more accessible.