Why choose Ochsner Health for your electrophysiology and heart rhythm disorders care?
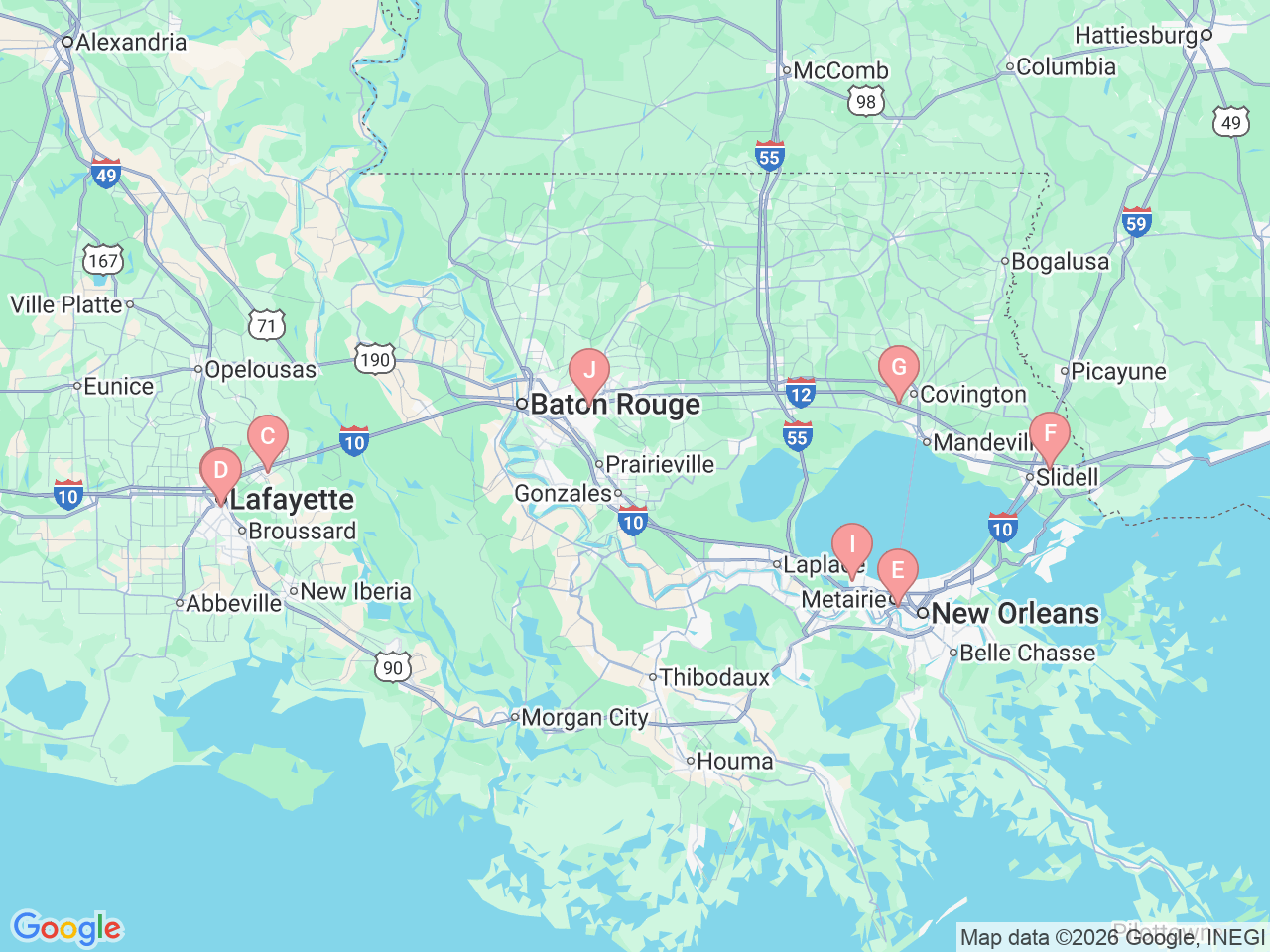
At Ochsner Health, exceptional care for electrophysiology and heart rhythm disorders is available in New Orleans, Kenner, Slidell, Covington, Baton Rouge, Lafayette and Breaux Bridge, Louisiana. Home to the largest electrophysiology laboratory space and the most diverse team of subspecialty experts in the Gulf South region, Ochsner has the expertise and resources to manage even the most complex heart rhythm conditions.
Our multidisciplinary team combines expertise with the latest advancements in treatment to provide personalized care for arrhythmias, atrial fibrillation and other heart rhythm disorders. With Ochsner, you don’t have to travel far for world-class care, it’s right here in your community.
Ochsner Health is the first in Louisiana to use Volta’s AI technology for atrial fibrillation (AFib) treatment, enhancing precision in catheter ablation procedures and improving patient outcomes.









-7abbbb2796.jpg)