Why choose Ochsner Health for your ventricular assist device?
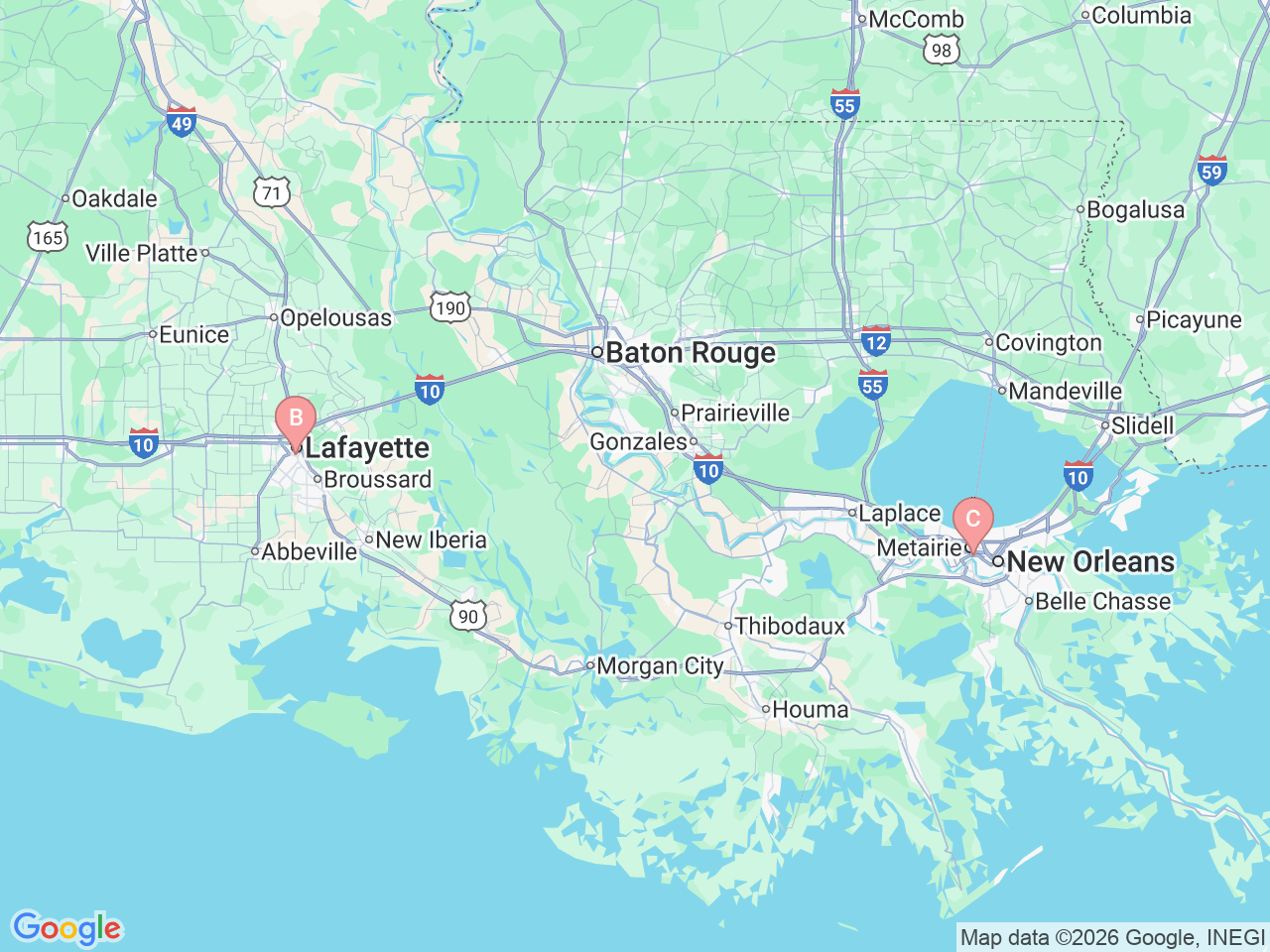
Ochsner Health offers interventional cardiology services in New Orleans and Lafayette, Louisiana, and is home to a comprehensive advanced heart failure program as well as one of the largest ventricular assist device (VADs) programs in the country. As the only VAD center in the Gulf South, Ochsner provides superior mechanical circulatory support treatments with exceptional outcomes, including:
- Performing 60 to 70 ventricular assist device implants annually
- Achieving a one-year survival rate of 98% for both bridge-to-transplant and destination therapy patients, with two- and three-year survival rates at 96%
- Receiving the Ventricular Assist Device Advanced Certification from The Joint Commission and designation from U.S. News & World Report as a “High Performing Hospital” for heart failure treatments, which includes ventricular assist devices
Whether you’re waiting for a heart transplant or seeking to improve your quality of life with late-stage heart failure, Ochsner Health is your trusted partner for ventricular assist device implantation.







-7abbbb2796.jpg)