Why choose Ochsner Health for your interventional cardiology care?
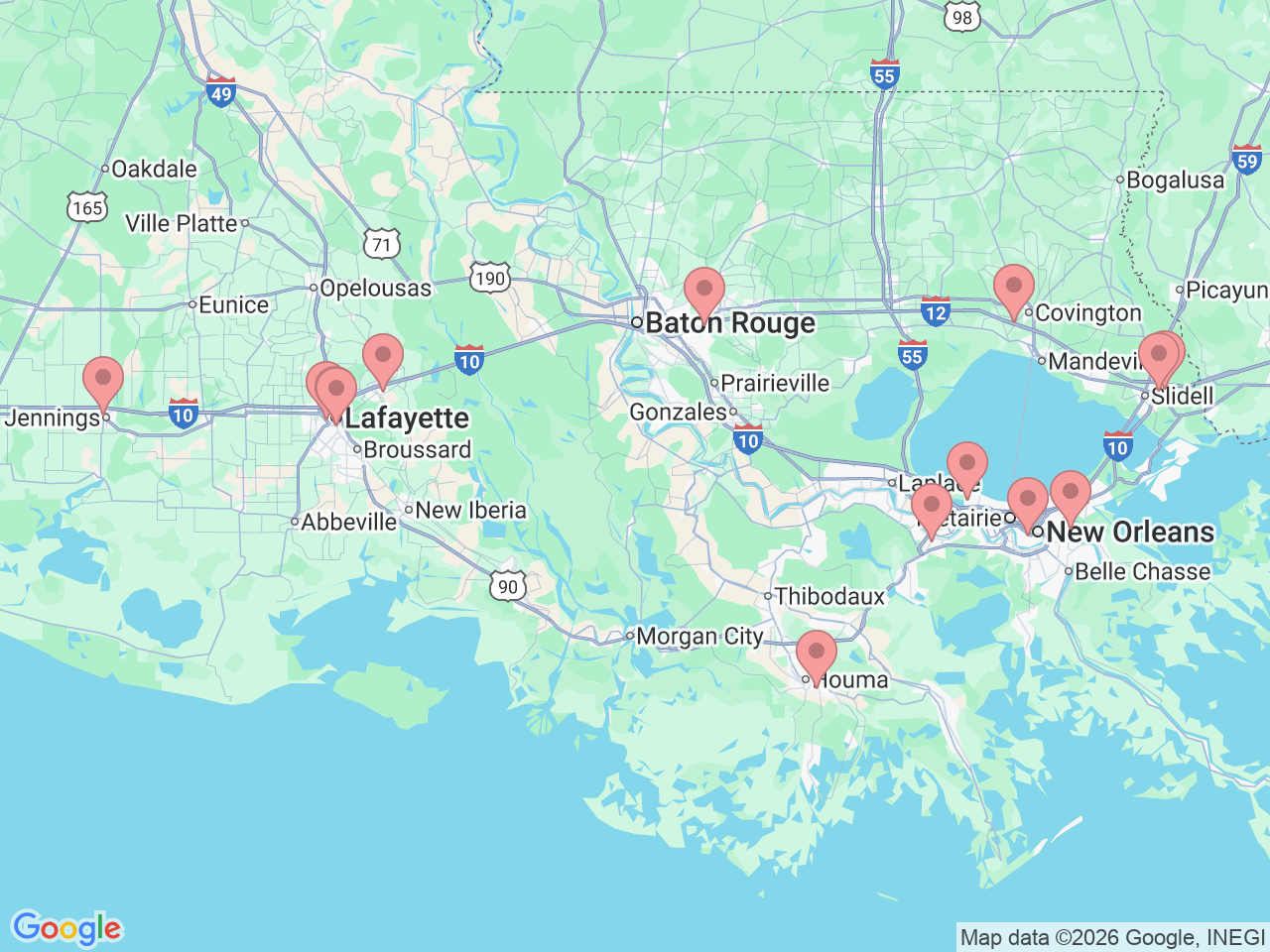
The John Ochsner Heart & Vascular Institute offers interventional cardiology services in New Orleans, Kenner, Baton Rouge, Slidell, Luling, Covington, Lafayette, Jennings, Breaux Bridge and Chalmette, Louisiana. Our interventional cardiology team is dedicated exclusively to interventional procedures, working alongside a multidisciplinary team of subspecialists to diagnose and treat conditions affecting the heart and blood vessels for patients across the Gulf South region.
Each year, our internationally recognized interventional cardiologists perform nearly 4,000 procedures, making them some of the most experienced in the nation. Our team includes national leaders from the American College of Cardiology, the Society for Cardiac Angiography and Interventions, and the Society of Vascular Medicine, all united by a shared mission: to provide nonsurgical treatments that prevent heart attacks, strokes, limb loss and structural heart disease.